Steroid-Induced Psychosis: How to Recognize and Treat It in an Emergency
 Dec, 15 2025
Dec, 15 2025
Steroid-Induced Psychosis Treatment Calculator
Calculate Appropriate Antipsychotic Dosing
Select the antipsychotic medication and symptom type to get recommended dose range.
Note: Always rule out other causes of psychosis before treating. Reduce steroid dose to < 40 mg prednisone daily as primary treatment. Do not use high doses of antipsychotics.
When someone starts taking high-dose steroids for asthma, lupus, or a flare-up of rheumatoid arthritis, they usually expect relief from swelling and pain. But in some cases, they might suddenly become confused, paranoid, or even hear voices. This isn’t a sign of weakness or a personal failing-it’s steroid-induced psychosis, a serious but treatable side effect that emergency teams need to spot fast.
What Exactly Is Steroid-Induced Psychosis?
Steroid-induced psychosis is a recognized medical condition listed in the DSM-5 as a substance/medication-induced psychotic disorder. It happens when corticosteroids-like prednisone, dexamethasone, or methylprednisolone-trigger delusions, hallucinations, or extreme mood swings that aren’t caused by another mental illness, drug use, or a physical brain problem.
It’s not rare. Studies show between 2% and 60% of people on high-dose steroids develop some kind of psychiatric symptom. The real danger zone? People taking more than 80 mg of prednisone per day. In one large study, nearly 1 in 5 patients on that dose developed clear psychotic symptoms. Even at 40 mg/day, over 4% of patients had noticeable changes in thinking or behavior.
These symptoms don’t show up after weeks. They usually hit within the first 2 to 5 days of starting the medication-or sometimes right after a dose increase. That’s why it’s so easy to miss. A patient might be admitted for pneumonia, get a high-dose steroid shot, and then suddenly start yelling about being watched by the government. Doctors might assume it’s delirium from infection, or worse, dismiss it as ‘just being dramatic.’ But if you don’t recognize it for what it is, you risk serious harm.
How Do You Spot It Early?
Waiting for full-blown hallucinations means you’ve already waited too long. The earliest signs are subtle but consistent:
- Confusion or trouble following simple conversations
- Unexplained agitation or restlessness
- Sudden mood swings-like going from calm to angry in minutes
- Difficulty sleeping, even when the body is exhausted
- Repeating the same thoughts or fears, even when told they’re not true
These aren’t just ‘bad days.’ They’re neurological reactions. Corticosteroids flood the brain with synthetic cortisol, which disrupts the balance between two key receptor systems: glucocorticoid and mineralocorticoid. This imbalance affects areas of the brain tied to emotion, memory, and perception-similar to what happens in Cushing’s syndrome or severe stress.
Research shows that mania (elevated mood, grandiosity, impulsivity) is more common in people on short-term, high-dose steroids. Depression, on the other hand, tends to appear after weeks or months of use. Psychosis-delusions and hallucinations-is less frequent than mood swings, but it’s the most dangerous because it increases the risk of violence, self-harm, or suicide.
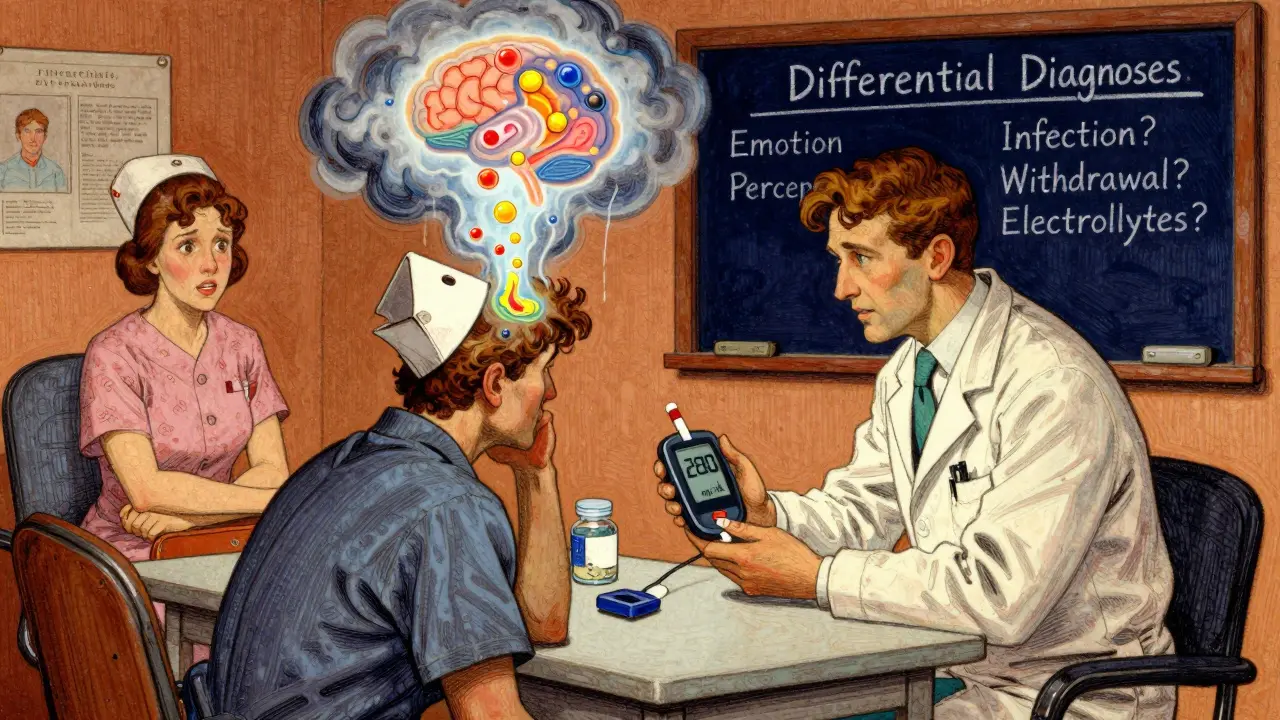
What Else Could It Be? Ruling Out Mimics
Before you label it steroid-induced psychosis, you have to rule out everything else. Many medical conditions look exactly like psychosis:
- High blood sugar from steroid-induced diabetes
- Low sodium or potassium from electrolyte shifts
- Brain infections like meningitis or encephalitis
- Drug interactions (especially with antidepressants or opioids)
- Alcohol or benzodiazepine withdrawal
- Underlying bipolar disorder or schizophrenia triggered by stress
That’s why every emergency evaluation needs the same basic checks:
- Ask: When did the steroids start? What’s the dose? Has it changed?
- Check: Blood glucose, electrolytes, kidney and liver function
- Test: Urine drug screen, CBC, CRP, TSH, vitamin B12
- Assess: Neurological exam-any tremors, weakness, or abnormal reflexes?
If the patient has a fever, neck stiffness, or altered consciousness, a lumbar puncture might be needed. If glucose is over 250 mg/dL, that could be the main driver of confusion. You can’t treat steroid psychosis until you’ve ruled out these mimics.
Emergency Treatment: Safety First, Then Medication
The first rule in any emergency psychosis: Do no harm. Physical restraints should be a last resort. They increase fear, raise cortisol further, and can cause injury. Instead, use calm verbal de-escalation. Lower lights, reduce noise, have one trusted person speak slowly and clearly.
If the patient is violent or poses a danger, sedation is needed. But here’s where most ER teams get it wrong-they reach for high doses of antipsychotics meant for schizophrenia. That’s dangerous.
For steroid-induced psychosis, lower doses work better and are safer:
- Olanzapine: 2.5-10 mg orally (not 20-30 mg)
- Risperidone: 1-2 mg orally or IM
- Haloperidol: 0.5-1 mg orally, or 2-5 mg IM (always give with diphenhydramine to prevent muscle spasms)
- Lorazepam: 1-2 mg IM if there’s severe anxiety or agitation
Studies show these doses resolve symptoms in 2-7 days. Higher doses don’t speed things up-they just cause more side effects like sedation, low blood pressure, or abnormal movements.
For patients who refuse pills, disintegrating tablets or IM injections are the best options. Avoid long-acting injectables like fluphenazine-they’re overkill and risky in this setting.
The Real Fix: Tapering the Steroids
Medication alone won’t cure this. The root cause is the steroid. The single most effective treatment? Reducing the dose.
Research shows that 92% of patients recover fully when their steroid dose is lowered to under 40 mg of prednisone per day-or the lowest possible dose needed for their underlying condition. That’s not a suggestion. It’s the standard of care.
But you can’t just stop steroids cold. Abrupt withdrawal can trigger adrenal crisis-low blood pressure, vomiting, shock, even death. The goal is to taper slowly while monitoring for both psychiatric symptoms and physical stability.
For example:
- If someone is on 120 mg prednisone daily, drop to 60 mg in 24-48 hours
- Then reduce by 10-20 mg every 2-3 days until under 40 mg
- Once stable, continue tapering under specialist supervision
If the patient needs the steroid for a life-threatening condition-like a severe flare of vasculitis or organ transplant rejection-then you manage the psychosis with antipsychotics while keeping the steroid dose as low as possible. That’s where collaboration with rheumatology or immunology is critical.

What About Lithium or Antidepressants?
Lithium can help prevent steroid-induced mania, especially in people with a history of bipolar disorder. But it’s not a first-line choice. It takes weeks to work, requires blood tests, and can cause kidney or thyroid damage. Only use it if antipsychotics fail and the patient is at high risk for mania.
Antidepressants like SSRIs? Sometimes used for steroid-induced depression, but they don’t help psychosis. Antiseizure drugs like valproate or carbamazepine? There’s weak evidence. They’re not recommended unless there’s a clear seizure risk or bipolar component.
The bottom line: Stick to low-dose antipsychotics and steroid tapering. Everything else is a backup plan.
Why Do So Many ER Doctors Get It Wrong?
A 2022 survey of 127 emergency physicians found that while 89% knew steroids could cause psychosis, only 43% consistently tapered the dose. Over 60% gave antipsychotics at doses meant for schizophrenia-sometimes 20-30 mg of olanzapine. That’s more than double what’s needed. It’s like using a sledgehammer to fix a loose screw.
Why? Lack of training. Most ER staff learn psychosis from schizophrenia cases, not medication-induced cases. They don’t realize steroid psychosis responds better to gentler treatment. The American College of Emergency Physicians updated its guidelines in 2023 to say: Use 50-75% less antipsychotic than you would for primary psychosis. But few ERs have protocols to enforce this.
What’s missing? Simple checklists. A one-page form asking: Did the patient start or increase steroids in the last 5 days? Are they confused or agitated? What’s their glucose and sodium? That’s all it takes to catch it early.
What’s Next? Better Tools Coming
The National Institutes of Health is running a study tracking 500 patients on high-dose steroids to find genetic or blood markers that predict who’s at risk. Early results suggest certain gene variants may make people more sensitive to cortisol’s effects on the brain.
By mid-2025, the American Psychiatric Association will release a clinical decision tool that helps doctors calculate risk based on steroid dose, age, past mental health history, and early symptoms. It’ll flag high-risk patients before psychosis even starts.
Until then, the best tool is awareness. If you’re prescribing or giving steroids, watch for the first signs. If you’re in the ER and someone looks ‘off’ after a steroid shot, don’t assume it’s ‘just anxiety.’ Ask the right questions. Order the right tests. Taper the steroid. Give the right dose of antipsychotic. You can save someone from weeks of suffering-and maybe even their life.
Can steroid-induced psychosis happen with low doses?
Yes, though it’s rare. Most cases occur with doses above 40 mg of prednisone per day. But people with a history of mental illness, older adults, or those with metabolic disorders can develop symptoms at lower doses. Never assume a dose is ‘too low’ to cause problems.
How long does steroid-induced psychosis last?
Symptoms usually improve within days of lowering the steroid dose and starting antipsychotics. Most patients recover fully in 1-3 weeks. If symptoms persist beyond 4 weeks, consider other causes like an underlying psychotic disorder that was triggered by the steroid.
Can you use benzodiazepines alone to treat it?
No. Benzodiazepines like lorazepam can help with agitation and anxiety, but they don’t treat delusions or hallucinations. They’re useful as an add-on, not a primary treatment. Relying on them alone delays proper care and can mask worsening symptoms.
Is steroid-induced psychosis permanent?
No. With prompt treatment, nearly all cases resolve completely. There’s no evidence it causes lasting brain damage. However, if untreated, the psychological trauma, hospitalization, or injury from psychosis can have long-term consequences.
Should patients avoid steroids forever after this?
Not necessarily. Many patients need steroids for chronic conditions. The key is to use the lowest effective dose, monitor closely, and have a plan in place. If psychosis happens again, doctors may switch to non-steroid alternatives like biologics or immunosuppressants. But steroids aren’t off-limits forever.

Sarthak Jain
December 15, 2025 AT 09:38bro i saw this happen to my uncle on 80mg prednisone after his lupus flare - thought he was just ‘going crazy’ till the ER doc asked if he’d been on steroids. he was yelling at the ceiling about ‘the nurses stealing his thoughts.’ wild. they dropped the dose and gave him 5mg olanzapine and he was back to normal in 3 days. why do docs always skip the steroid question? like, it’s right there in the chart.
Jonny Moran
December 17, 2025 AT 06:39As a med student rotating through the ER last year, this is 100% spot on. We had a patient on 120mg prednisone for vasculitis who started talking to the IV pole like it was his therapist. Everyone assumed it was sepsis-induced delirium until someone checked the med list. Tapered him down to 40mg, gave 2mg risperidone IM, and within 18 hours he was asking for pizza. The real tragedy? He’d had this exact same episode 2 years prior and no one documented it. We need checklists. Like, now.
Daniel Wevik
December 18, 2025 AT 12:36Let me cut through the noise: steroid psychosis isn’t ‘rare’ - it’s underdiagnosed because we’re trained to see schizophrenia, not iatrogenic reactions. The dose-response curve is nonlinear. At 40mg, you’re looking at 4% incidence. At 80mg, it’s 20%. That’s not a fluke, that’s a pharmacokinetic grenade. And no, you don’t need lithium. You need to reduce the steroid and give 5mg olanzapine max. High-dose antipsychotics just add EPS risk and prolong sedation. This isn’t psychiatry 101 - it’s clinical pharmacology 101.
Rich Robertson
December 20, 2025 AT 04:34Just wanted to add - this happens more than people think in the ICU too. We had a post-op patient on methylprednisolone for ARDS who started believing his ventilator was a spy device. We missed it for 12 hours because he was ‘stable’ otherwise. Glucose was 310, sodium was 130 - classic steroid triad. Once we dropped the steroid and corrected electrolytes, the psychosis lifted like a fog. Bottom line: if they’re on high-dose steroids and acting weird, check labs before you reach for Haldol.
Dwayne hiers
December 20, 2025 AT 19:11Correcting a misconception: the 2–60% range cited in literature is misleading because it includes all psychiatric symptoms - anxiety, insomnia, mood lability. True psychosis (delusions/hallucinations) occurs in 5–15% of patients on >80mg/day. The DSM-5 criteria are clear: symptoms must not be better explained by another disorder. Always rule out metabolic derangements first - hyperglycemia alone can mimic psychosis. Also, lorazepam is not a substitute for antipsychotics. It may reduce agitation but does nothing for positive symptoms. And yes - tapering is the definitive treatment. Antipsychotics are a bridge, not a cure.
jeremy carroll
December 22, 2025 AT 03:31my grandma got this after her knee surgery - they gave her a 120mg shot and she started crying at the TV saying the actors were talking to her. we thought she was just confused from pain meds. turned out it was the steroid. doc tapered her down and gave her a tiny bit of risperidone. she’s fine now. just wanted to say - this stuff happens to normal people, not just ‘crazy’ folks. please listen to your patients. they know something’s off.
Daniel Thompson
December 23, 2025 AT 22:42Interesting. But have you considered the role of cortisol receptor polymorphisms? Recent studies suggest that individuals with NR3C1 gene variants exhibit heightened sensitivity to exogenous glucocorticoids, leading to disproportionate limbic system dysregulation. Furthermore, the gut-brain axis may be modulated by steroid-induced microbiota shifts, potentially exacerbating neuroinflammation. Without controlling for these confounders, the causal attribution remains speculative. This is why we need longitudinal neuroimaging studies - not just checklists.
Alexis Wright
December 24, 2025 AT 10:14Let’s be real - this entire post is just a glorified drug company pamphlet. The real issue? Steroids are overprescribed because they’re cheap and fast. Doctors don’t care about psychosis because they’re paid for procedure volume, not patient outcomes. You think they’re gonna taper a 120mg dose when the rheumatologist wants it at 80mg for ‘control’? Nope. They’ll just slap on 20mg of olanzapine and call it a day. And the NIH study? It’s funded by Pfizer. They want to patent a genetic test so they can charge $2,000 for ‘risk stratification.’ Wake up. This isn’t medicine. It’s profit-driven triage disguised as science.