Rationing Medications: How Ethical Decisions Are Made During Drug Shortages
 Dec, 1 2025
Dec, 1 2025
When a life-saving drug runs out, who gets it? This isn’t science fiction. It’s happening right now in hospitals across the U.S., Australia, and beyond. In 2023, the FDA listed 319 active drug shortages-up from just 61 in 2005. Some of the most critical shortages hit cancer drugs like carboplatin and cisplatin, leaving oncologists to choose between patients who both need the same treatment. No one wants to play God. But when supplies vanish, someone has to decide-and that decision can’t be left to chance.
Why Medication Rationing Is Happening Now
Drug shortages aren’t random. They’re the result of broken supply chains, manufacturing failures, and market consolidation. Three companies produce 80% of generic injectable drugs in the U.S., meaning if one plant shuts down, dozens of hospitals lose access. In 2023, 87% of community oncology clinics reported severe shortages of platinum-based chemotherapy drugs. Academic centers fared slightly better, but even they weren’t immune. The problem isn’t just scarcity-it’s timing. A drug shortage can go from mild to critical in weeks. Hospitals don’t have months to prepare. They’re often caught off guard. That’s when bedside decisions happen. A nurse gives the last vial to the patient in Room 307 because they’re younger. A doctor delays treatment for someone with metastatic cancer because they think the other patient has a better shot. These aren’t policy decisions. They’re survival instincts-and they’re unfair.What Ethical Rationing Actually Looks Like
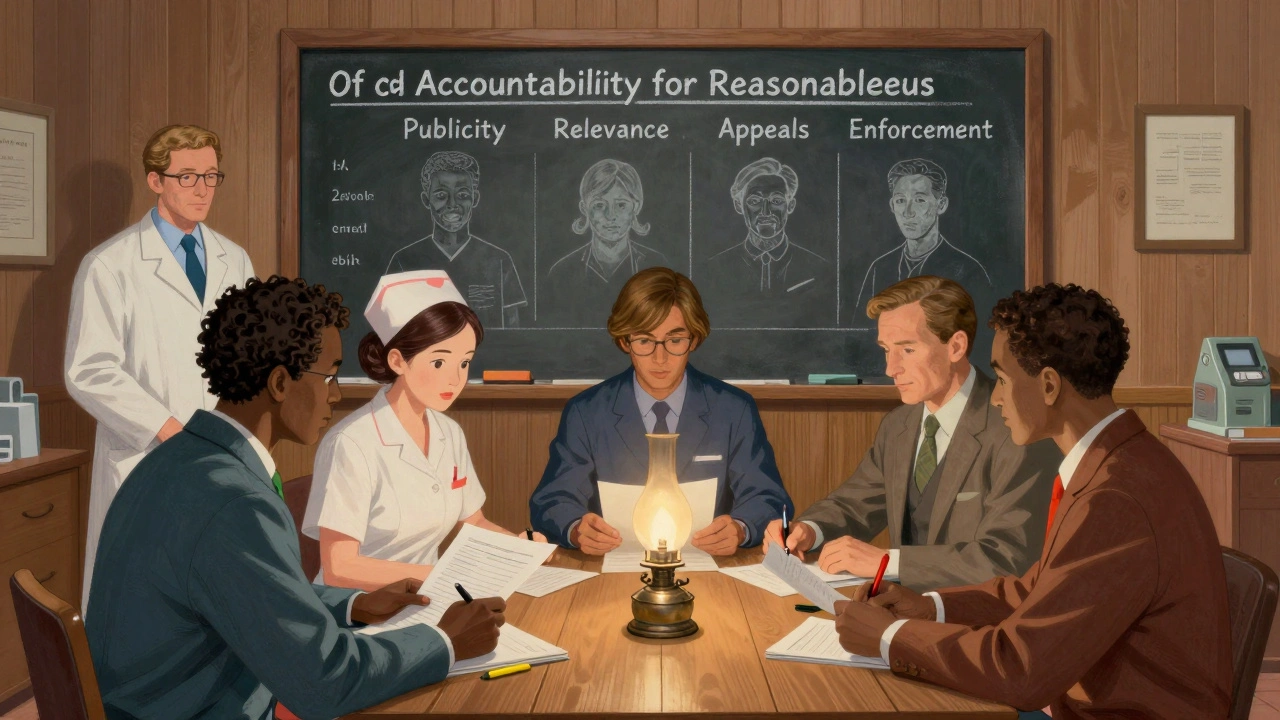
Ethical rationing doesn’t mean picking patients based on gut feeling. It means using clear, agreed-upon rules so no one is left to guess who deserves care. The most respected framework comes from Daniels and Sabin’s “Accountability for Reasonableness.” It’s not about who lives or dies. It’s about how the decision is made. There are four pillars:- Publicity: Everyone-patients, staff, families-must know how decisions are made.
- Relevance: Criteria must be based on medical evidence, not bias. For example, prioritizing patients with curative intent over palliative care.
- Appeals: If a patient or family disagrees, there’s a way to challenge the decision.
- Enforcement: Someone has to make sure the rules are followed.
How Criteria Are Applied in Real Cases
In Minnesota, when carboplatin ran out in 2023, they didn’t just say “give it to the sickest.” They built a tiered system:- Tier 1: Patients receiving treatment with curative intent, no equally effective alternative.
- Tier 2: Patients with high recurrence risk and no other options.
- Tier 3: Palliative care patients or those with alternatives.
- How many years of life are saved?
- Will this drug give the patient meaningful time?
- Is the patient a healthcare worker? (Some frameworks prioritize frontline staff to keep the system running.)
The Human Cost of Poor Rationing
Behind every shortage is a story of moral injury. One oncologist in Ohio told a JAMA survey: “I had to choose between two stage IV ovarian cancer patients for the last dose of carboplatin. I picked the one with the better lab results. I didn’t tell either one why.” That’s not rare. Only 36% of patients are told they’re being rationed. Families assume the drug isn’t working. They don’t know it’s gone. Clinicians feel guilty. Burnout rates jump 27% when decisions are made alone. A 2022 Mayo Clinic study found hospitals with ethics committees had 41% lower burnout scores. And then there’s the hidden inequity. A 2021 report found 78% of rationing protocols don’t include any measure to protect marginalized groups-Black, Indigenous, low-income, or rural patients. These are the same people who already face longer wait times and fewer specialists. When drugs are scarce, they’re often last in line.What Works: Real Examples of Success
Not all hospitals are flying blind. At a large teaching hospital in Chicago, they created a Drug Shortage Response Team in 2022. It met every Monday. They tracked inventory in real time. They trained staff on communication scripts. They used a digital dashboard that flagged when a drug was down to 72 hours of supply. When cisplatin ran low, they didn’t panic. They called the committee. They reviewed each case against the tiers. They notified patients in writing. They offered alternatives-like switching to carboplatin if safe-or clinical trials. They documented every decision. Within six months, clinician distress dropped by 52%. Another hospital in Minnesota started a “conservation-first” policy. Instead of giving full doses, they used the lowest effective dose at the longest possible interval. For some patients, that meant cutting from weekly to every three weeks. It wasn’t ideal-but it stretched the supply by 40% and saved lives.
What’s Missing-and What’s Coming
The biggest gap? Standardization. Every hospital does it differently. One uses age. One uses survival probability. One uses who’s been waiting longest. That’s chaos. The National Academy of Medicine is working on national standards, with draft criteria expected in early 2024. The FDA is launching an AI-powered early warning system to predict shortages before they happen-targeting a 30% reduction in duration by 2025. But technology alone won’t fix ethics. What’s needed is training. A 2023 CDC toolkit recommends 8 hours of ethics education for all staff involved in rationing. Only 13% of hospitals currently offer it. And patients? They need to be part of the conversation. ASCO now requires hospitals to document whether patients were informed. That’s a start. But transparency means more than a note in a chart. It means having a real conversation-about risk, hope, and limits.What You Can Do
If you’re a patient or family member: ask. If you’re told a drug isn’t available, ask why. Ask if there’s a plan. Ask if others are getting it. You have a right to know. If you’re a healthcare worker: push for a committee. Advocate for training. Document your decisions. Don’t make them alone. If you’re a policymaker: fund the infrastructure. Require transparency. Hold manufacturers accountable. The 2012 law requiring early shortage notices is ignored by 32% of companies. That’s not a loophole-it’s a failure. Rationing isn’t about choosing who lives. It’s about making sure no one dies because the system failed them.Is medication rationing legal?
Yes, but only when done ethically and transparently. In the U.S., rationing isn’t illegal-it’s unregulated. Hospitals can’t refuse care outright, but they can prioritize based on medical need if they follow established frameworks like Daniels and Sabin’s. The key is consistency, documentation, and patient communication. Without those, rationing becomes discrimination.
Are there alternatives to rationing drugs?
Yes. The first step is conservation: using the smallest effective dose, extending dosing intervals, or switching to similar drugs. The second is substitution: using non-injectable forms or newer therapies. The third is prevention: building backup supply chains, supporting multiple manufacturers, and investing in domestic production. Rationing should be the last resort, not the default.
Why aren’t more hospitals using ethical committees?
Because they’re hard to set up. It takes time, money, and leadership buy-in. Many hospitals don’t have ethicists on staff. Others fear legal liability. Some think it’s overkill-until they’re forced to make a life-or-death call without a plan. A 2022 survey found only 2.8% of hospitals included ethicists in their shortage teams. Most still rely on the on-call doctor, who’s often exhausted and untrained.
Do patients ever get angry about rationing?
Yes. In 2021, the Patient Advocate Foundation recorded 127 formal complaints about undisclosed rationing. Patients felt lied to, abandoned, or punished. The anger isn’t just about losing treatment-it’s about being kept in the dark. When hospitals communicate clearly and involve patients in the process, complaints drop by over 60%.
Can I request a specific drug if it’s in short supply?
You can ask, but you can’t demand it. If a drug is rationed, hospitals must apply the same rules to everyone. Asking for a specific drug isn’t wrong-it’s human. But if the hospital has a tiered system, your request will be evaluated against clinical criteria, not personal preference. The goal is fairness, not favoritism.
What’s being done to prevent future shortages?
The FDA is building an AI-based early warning system to predict shortages before they happen. The National Academy of Medicine is creating standardized ethical allocation metrics. Some states are passing laws to require hospitals to report shortages and rationing practices. But the biggest fix? Reducing market consolidation. Right now, three companies control 85% of generic injectables. More competition means less risk of total supply collapse.

Gene Linetsky
December 2, 2025 AT 19:15This is all just corporate greed dressed up as ethics. Three companies control 80% of injectables? That’s not a coincidence-that’s a cartel. The FDA knows this and does nothing. They’re paid off. You think they care about your cancer? They care about quarterly profits. Wake up.
Archie singh
December 3, 2025 AT 18:57Accountability for Reasonableness sounds nice on paper but it’s just bureaucratic theater. Ethics committees don’t make drugs appear. They just make doctors feel better while patients die slowly. The real problem isn’t ethics-it’s supply chain collapse. Fix the system or stop pretending you’re moral.
Jim Schultz
December 4, 2025 AT 09:29Let’s be real: if you’re not on a tier-1 list, you’re basically being told you’re expendable. And who gets to define 'curative intent'? A committee of people who’ve never held a dying patient’s hand? This isn’t medicine-it’s actuarial science with a side of guilt. And don’t even get me started on the 78% of protocols that ignore race and class. It’s eugenics with a PowerPoint.
Gavin Boyne
December 4, 2025 AT 23:29Here’s the uncomfortable truth: we’ve outsourced moral responsibility to algorithms and committees because we’re too scared to own our choices. But no framework can absolve a human of the weight of deciding who lives. That’s not policy-that’s sacred ground. And we’re treating it like an HR流程.
Kidar Saleh
December 6, 2025 AT 00:10In the UK, we don’t have this problem because we have universal healthcare. But even here, when drugs are scarce, it’s the elderly, the poor, and migrants who suffer most. This isn’t about medical criteria-it’s about who society values. And right now, the answer is: not enough.
Chloe Madison
December 6, 2025 AT 09:10I’ve worked in oncology for 12 years. I’ve seen nurses cry after giving the last vial to a 12-year-old because their mom begged them to. This isn’t just about protocols-it’s about trauma. We need mandatory mental health support for staff, not just another checklist. Your soul doesn’t get a bonus for doing the right thing when the system fails.
Katherine Gianelli
December 7, 2025 AT 04:43My cousin got denied cisplatin because she was 'palliative'-but she was the one who cooked for everyone, who showed up to every chemo with cookies and jokes. They didn’t know her. They just saw a chart. That’s the real tragedy-not the shortage, but how we reduce people to numbers while pretending we’re being fair.
parth pandya
December 8, 2025 AT 13:11India also face this problem but we dont have good data. Many hospital just give drug to who pay more or who have connection. Ethical framework? What is that? We need more generic drug factory not more committee
Rashi Taliyan
December 9, 2025 AT 15:18As someone who lost a parent to delayed treatment during a shortage, I can tell you: silence is violence. If a hospital doesn’t tell you why you’re not getting the drug, they’re not just failing-they’re betraying you. Transparency isn’t optional. It’s dignity.
Kara Bysterbusch
December 9, 2025 AT 18:27Imagine if we treated drugs like we treat water or electricity-infrastructure, redundancy, public investment. Instead, we treat them like luxury goods. We’ve normalized scarcity because profit > humanity. The real scandal isn’t the shortage-it’s that we accept it.
Rashmin Patel
December 10, 2025 AT 12:42Look, I get the frameworks, I get the committees, but here’s what no one says: sometimes the person who needs it most is the one who can’t scream the loudest. I work with rural families who don’t even know how to ask for a second opinion, let alone challenge a rationing decision. If your system only works for people who know how to navigate bureaucracy, then it’s not ethical-it’s elitist.
sagar bhute
December 12, 2025 AT 05:27Another feel-good article from people who’ve never had to choose between two patients. You think your tiered system is fair? It’s just a mask for the same old bias. Who decides who has 'curative intent'? The same doctors who hate treating uninsured patients? Please. This is moral theater. The real solution? Nationalize pharmaceuticals. Or stop lying.
Cindy Lopez
December 13, 2025 AT 16:14So… what’s the point of this? We already know it’s broken. Why write a 3000-word essay?
Albert Essel
December 14, 2025 AT 17:31What if we stopped thinking of rationing as a crisis and started seeing it as a design flaw? We don’t ration air or water in emergencies-we build systems to ensure access. Why treat drugs differently? Maybe the answer isn’t more committees, but more manufacturing, more competition, and less profit-driven consolidation.
Ignacio Pacheco
December 15, 2025 AT 10:31So let me get this straight: we’ve got AI predicting shortages, ethics committees deciding who lives, and yet 64% of hospitals still rely on whoever’s on call at 3am? That’s not innovation. That’s a farce. You’re building a spaceship while using horse-drawn carts to deliver the fuel.