Peptic Ulcer Disease: What Causes It and How Antibiotics and Acid Reducers Fix It
 Dec, 25 2025
Dec, 25 2025
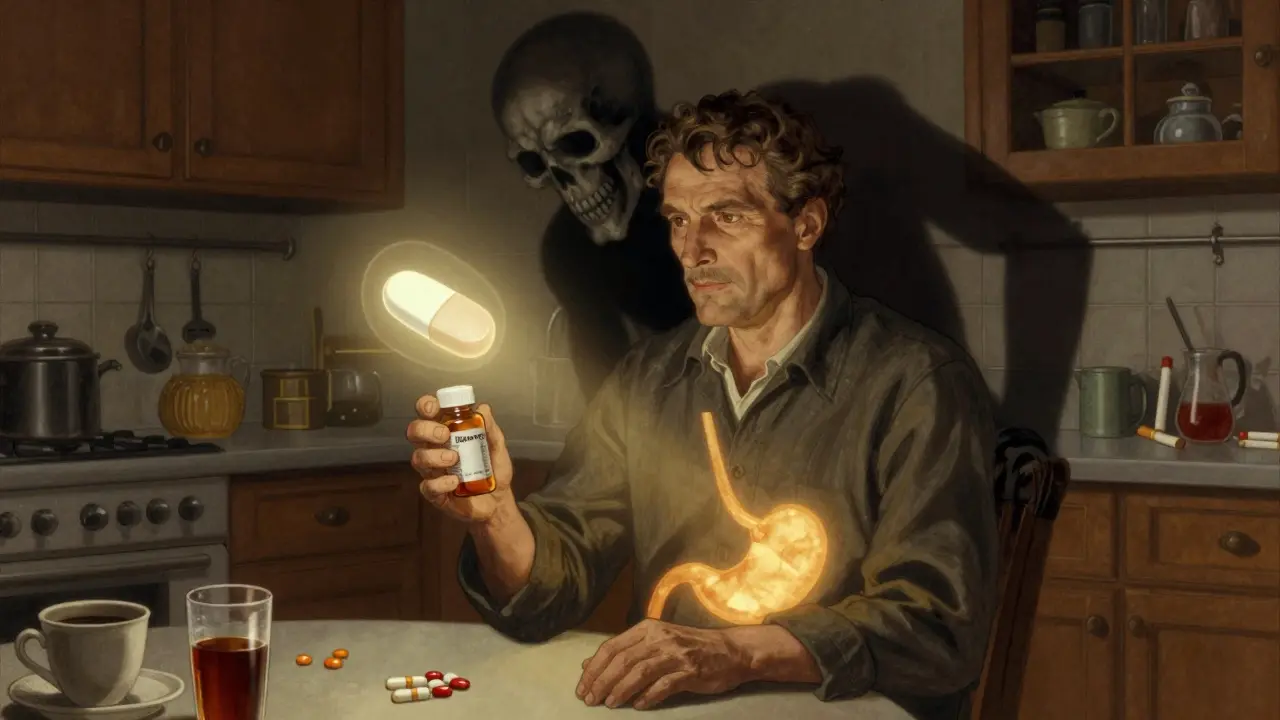
Most people think stomach ulcers are caused by stress or spicy food. That’s what we were told for decades. But here’s the truth: peptic ulcer disease is mostly caused by a bacteria you can’t see and painkillers you probably take without thinking. And the good news? It’s one of the most treatable conditions in gastroenterology-if you know what to do.
What Actually Causes a Peptic Ulcer?
A peptic ulcer isn’t just a sore in your stomach. It’s a deep break in the lining of your stomach or the first part of your small intestine (duodenum). This lining normally protects itself from stomach acid. But when that protection fails, acid eats through, causing pain, bleeding, and sometimes serious complications. There are two main culprits. The first is Helicobacter pylori (H. pylori), a spiral-shaped bacteria that lives in the stomach. It was discovered in 1982 by two Australian doctors, Barry Marshall and Robin Warren, who proved it wasn’t just a bystander-it was the cause. They even drank a culture of it to prove their theory. Marshall got sick. They won the Nobel Prize in 2005. Today, H. pylori is found in over half of all duodenal ulcers and 30-50% of gastric ulcers. The second major cause? NSAIDs. That’s nonsteroidal anti-inflammatory drugs: ibuprofen, naproxen, aspirin. These are the go-to painkillers for headaches, back pain, arthritis. But they block protective chemicals in the stomach lining. In fact, NSAIDs now cause more ulcers than H. pylori in many places, especially among older adults who take them daily. If you’re over 60 and take ibuprofen every day for knee pain, you’re at higher risk. Stress and spicy food? They don’t cause ulcers. But they can make them worse. Smoking doubles or triples your risk. Drinking more than three alcoholic drinks a day increases it by 300%. So while they’re not the root cause, they’re still dangerous partners in crime.How Do You Know You Have One?
The classic sign is a burning or gnawing pain in your upper belly, right below the breastbone. It often comes between meals or at night. Some people say it feels better after eating-then comes back a couple hours later. That’s because food temporarily buffers the acid against the ulcer. Other signs include:- Feeling full too fast
- Nausea or vomiting
- Intolerance to fatty or greasy foods
- Bloating or belching
Antibiotics: How They Erase H. pylori
If H. pylori is the cause, antibiotics are the solution. But not just one. You need a combo. The old standard was triple therapy: two antibiotics plus a proton pump inhibitor (PPI) for 7-14 days. Common combinations include:- Amoxicillin + clarithromycin + omeprazole
- Metronidazole + clarithromycin + lansoprazole
- Amoxicillin + metronidazole + pantoprazole
Acid-Reducing Medications: PPIs vs. H2 Blockers
Antibiotics kill the bacteria. But acid-reducing meds give your stomach time to heal. That’s where proton pump inhibitors (PPIs) come in. PPIs like omeprazole (Prilosec), esomeprazole (Nexium), pantoprazole (Protonix), and lansoprazole (Prevacid) block the final step of acid production. One dose lasts 24-72 hours. That’s why they’re the gold standard. They heal ulcers faster than anything else. H2 blockers-like famotidine (Pepcid), cimetidine (Tagamet), and nizatidine (Axid)-work too, but they’re weaker. They only block about half the acid and last 10-12 hours. They’re fine for mild heartburn, but not for healing ulcers. Timing matters. PPIs must be taken 30-60 minutes before a meal. That’s when your stomach’s acid pumps are waking up. Take them after eating? They’re less effective. But there’s a catch. Long-term PPI use has risks. The FDA has issued warnings about:- Increased risk of bone fractures with high doses over a year
- Lower vitamin B12 levels (because acid helps absorb it)
- Higher chance of C. difficile infection (a serious gut bug)
- Rebound acid hypersecretion-your stomach overproduces acid when you stop
What If You Need NSAIDs?
If you have arthritis, back pain, or heart disease and need daily NSAIDs, you can’t just stop. So what do you do? Option one: switch to COX-2 inhibitors like celecoxib (Celebrex). They’re gentler on the stomach, but not risk-free. Option two: take a PPI daily as a shield. Many doctors prescribe this long-term for high-risk patients. There’s also misoprostol, a prostaglandin analog. It helps rebuild the stomach lining. But it’s not popular-it causes cramping and diarrhea. And if you’re a woman of childbearing age? It can cause miscarriage. So it’s rarely used. The best move? Use the lowest effective NSAID dose for the shortest time. And always pair it with acetaminophen (Tylenol) when you can. It doesn’t hurt your stomach.
Lifestyle: The Silent Healer
Medicines fix the problem. But your habits keep it from coming back.- Quit smoking. Smokers heal slower. Their ulcers are more likely to bleed. Smoking cuts blood flow to the stomach lining-exactly what you don’t want.
- Limit alcohol. More than three drinks a day triples your risk. Even moderate drinking can irritate an already damaged lining.
- Don’t self-medicate. Over-the-counter painkillers are not harmless. Read labels. Don’t take multiple NSAIDs at once.
- Manage stress. It won’t cause an ulcer, but it can make pain feel worse and slow healing.
What Happens After Treatment?
After finishing your antibiotics and PPI, you’ll need a follow-up test. Not because you feel bad. Because you might still have H. pylori. The breath test or stool test is the gold standard for confirmation. Don’t skip it. Up to 20% of people don’t clear the infection on the first try. If the ulcer doesn’t heal? That’s called a refractory ulcer. It’s usually because:- You didn’t take the meds correctly
- The bacteria are resistant
- You’re still taking NSAIDs
- You’re still smoking

Jay Ara
December 26, 2025 AT 09:33so h pylori is the real villain huh? i always thought spicy food did it... mind blown
josue robert figueroa salazar
December 27, 2025 AT 13:56lol another medical article pretending to be revolutionary. we knew about h pylori in the 90s. why is this even trending?
Michael Bond
December 28, 2025 AT 22:02antibiotics + ppi works. simple. effective. stop overcomplicating it.
carissa projo
December 30, 2025 AT 01:31the body is not a machine to be fixed with chemicals-it’s a living ecosystem. h pylori isn’t just a pathogen-it’s a ghost of our ancestral microbiome, and we’ve been chasing it with brute force while ignoring the soil our gut is planted in. healing isn’t eradication-it’s restoration. when we treat the terrain instead of just the symptom, the bacteria lose their foothold without needing to kill them. ppi’s silence the fire but don’t heal the hearth.
what if the real problem isn’t the bacteria-but the modern diet, the chronic stress, the silent dehydration of our mucosal lining? we’ve been taught to fear microbes, not to listen to them.
and yet… i still take my amoxicillin. because i’m human. and fear is louder than philosophy.
christian ebongue
December 31, 2025 AT 20:40so you’re telling me i’ve been taking ibuprofen for my back pain like a dumbass and now i gotta take 4 pills twice a day just to not bleed out? thanks doc
Jody Kennedy
January 2, 2026 AT 13:39you’re not alone. i took ppi for 3 years. stopped cold turkey. woke up feeling like my stomach was on fire. turned out it was rebound acid. took me 6 weeks to taper off. now i drink aloe juice and chill. no meds. no panic.
Joanne Smith
January 3, 2026 AT 15:07vonoprazan sounds like a sci-fi drug name. next thing you know we’ll have nano-bots that whisper to h pylori and convince it to leave peacefully.
also-why does everyone act like misoprostol is the devil? it’s just a prostaglandin. it doesn’t care if you’re a woman. it just wants to heal your mucosa. if you’re preggo? don’t take it. duh.
jesse chen
January 4, 2026 AT 13:37Can you believe that Marshall and Warren drank the bacteria? That’s like… next-level dedication. I mean, who does that? I’d be Googling ‘how to disinfect a glass’ before even thinking about it. And they won a Nobel Prize for it? That’s the kind of bravery we need more of-science with guts. Literally.
Prasanthi Kontemukkala
January 6, 2026 AT 09:01in india, we’ve always used turmeric and honey for stomach pain. not sure if it kills h pylori but it sure calms the burn. maybe science should look at traditional remedies before inventing new pills.
Alex Ragen
January 7, 2026 AT 17:12Oh, so now we’re romanticizing ancient wisdom while ignoring the fact that H. pylori causes gastric cancer? And you’re telling me to ‘listen’ to a bacterium that evolved to exploit our stomach lining? That’s not philosophy-that’s dangerous pseudoscience dressed in incense.
Let me guess: you also think vaccines are ‘toxins’ and that fluoride is a ‘government mind-control agent’?
Sarah Holmes
January 8, 2026 AT 19:12How dare you suggest that modern medicine is anything less than divine intervention? You speak of turmeric and honey as if they are equal to proton pump inhibitors-this is not a yoga retreat, it is a battlefield of biochemistry. The Nobel laureates did not risk their lives so that we could return to the age of herbal teas and wishful thinking. Your ‘ecosystem’ nonsense is a luxury of the privileged who have never felt the searing agony of a perforated ulcer. Take your pills. Be grateful. And stop turning science into a spiritual quest.
david jackson
January 9, 2026 AT 20:20Okay, but imagine this: you’re a bacterium living in a human stomach. For millions of years, you coexisted peacefully. Then, boom-modern diets, antibiotics, stress, NSAIDs, processed food, sleep deprivation, caffeine, alcohol, smoking, blue light, existential dread-you name it. Suddenly, you’re not just surviving, you’re fighting for your entire lineage’s existence. And now humans are treating you like a terrorist? You’re not evil-you’re just trying to survive in a world that turned your home into a warzone. What if the real villain isn’t H. pylori… but the way we’ve broken our own biology? What if healing isn’t about killing the enemy, but rebuilding the house they were forced to live in?
And vonoprazan? That’s not a drug. That’s a god. A silent, chemical deity that shuts down acid like a cosmic off-switch. I don’t know if I should be terrified or in awe.
Also, I just took my last PPI yesterday. My stomach is whispering. I think it’s saying thank you.