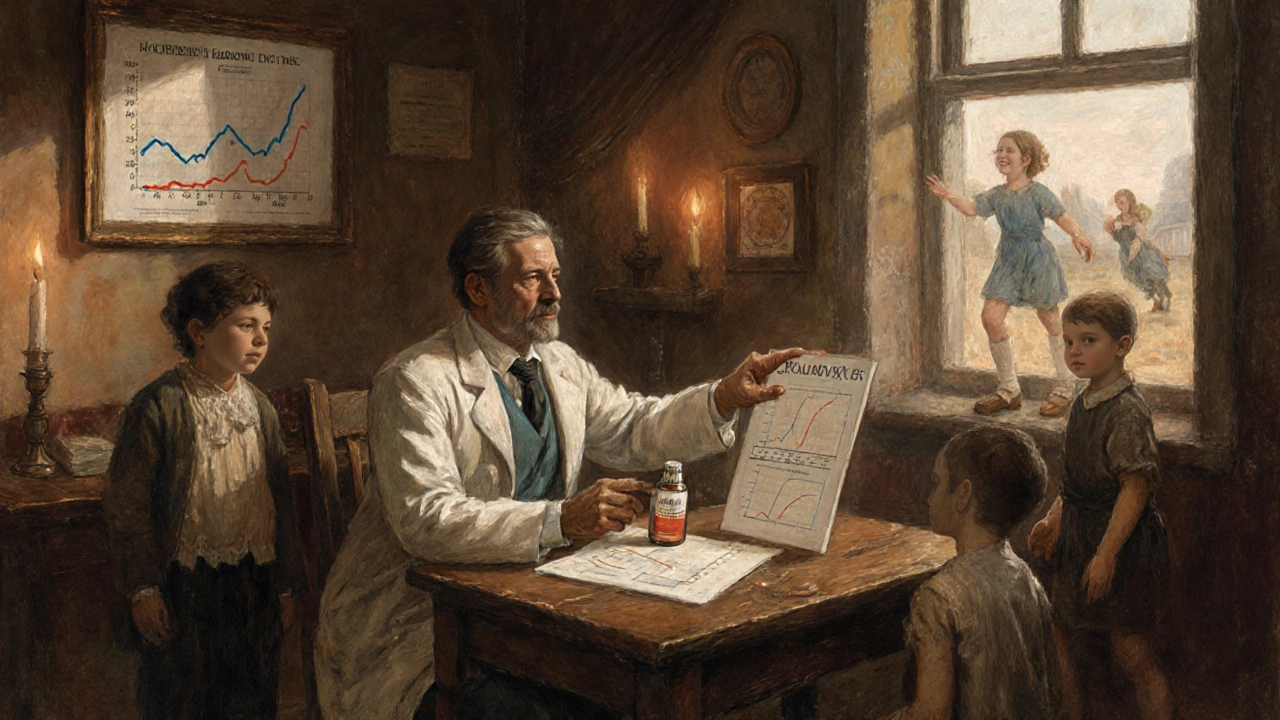
Pain Medications: Opioids vs Non-Opioids - What’s Safe and What’s Not
 Nov, 14 2025
Nov, 14 2025
When you hurt - whether it’s a bad back, a sore knee, or pain after surgery - you want relief. Fast. But not all pain meds are created equal. And the choice between opioids and non-opioids isn’t just about how strong they are. It’s about risk. The kind of risk that can change your life - or end it.
What Are Opioids, Really?
Opioids are drugs like oxycodone, hydrocodone, morphine, and fentanyl. They work by locking onto special receptors in your brain and spinal cord to block pain signals. They’re powerful. And for some people - like those with advanced cancer or severe trauma - they’re necessary.
But for most chronic pain conditions - lower back pain, osteoarthritis, headaches - opioids don’t work better over time than simpler options. In fact, the SPACE trial, which followed 240 people with chronic pain for a full year, found no difference in how well people could function between those taking opioids and those taking non-opioids like ibuprofen or acetaminophen. The opioid group even reported slightly worse pain levels.
And here’s the scary part: long-term use raises your risk of heart attack. A study of nearly 300,000 patients showed that if you’re on opioids for 180 days or more over three years, your chance of having a heart attack jumps by more than 160%. Daily doses above 120 mg of morphine equivalent? That’s a 58% higher risk compared to low or no use.
Why Non-Opioids Are Often the Better Choice
Non-opioid pain relievers include NSAIDs like ibuprofen and naproxen, acetaminophen (Tylenol), and newer options like Journavx, approved by the FDA in March 2024. These don’t target the brain’s reward system. They don’t cause euphoria. And they don’t lead to addiction.
For acute pain - like after a dental procedure or a broken bone - studies in children show non-opioids work just as well. One study compared morphine to ibuprofen in kids with fractures. Pain scores were nearly identical. But the morphine group had way more nausea, vomiting, drowsiness, and even low oxygen levels. Another study found over half of kids on codeine or tramadol had nausea or constipation. No one needed stronger pain control. Just safer options.
The VA’s own research says it plainly: opioids weren’t more effective than non-opioids for chronic pain - but they came with far more side effects. Dizziness. Constipation. Confusion. Falls. And yes, addiction.
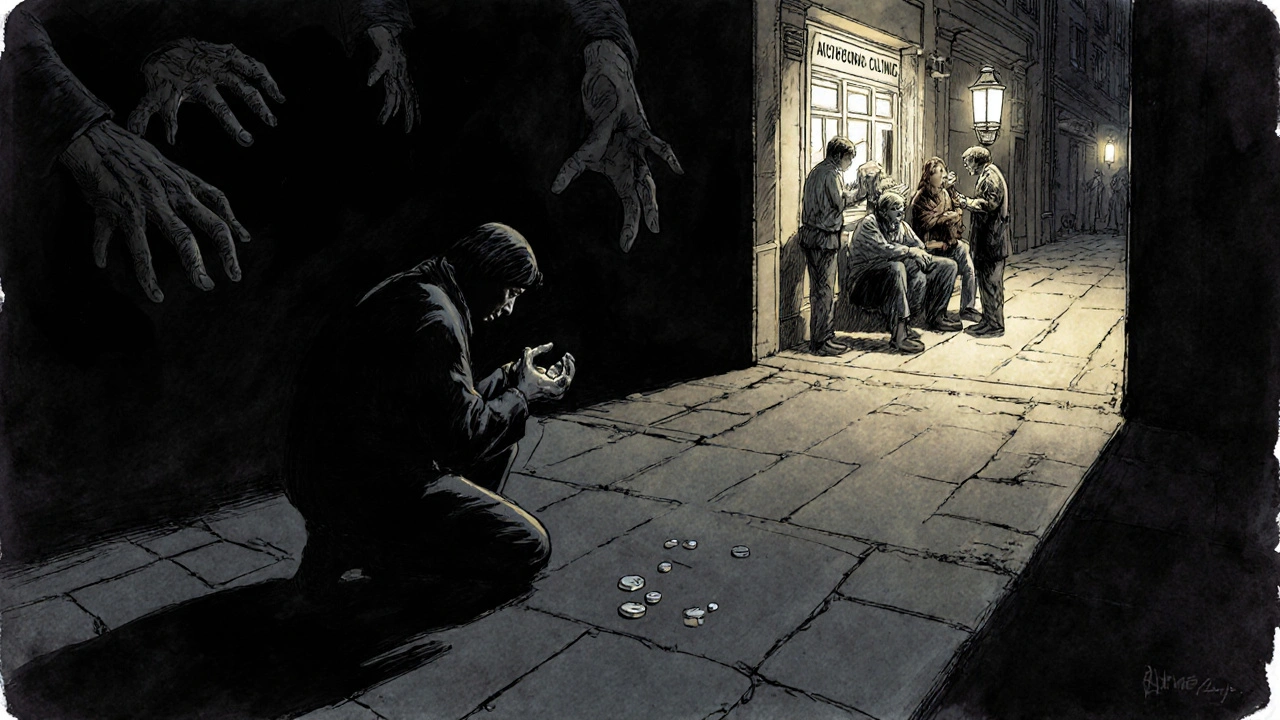
The Opioid Epidemic Isn’t Over
In 2021, over 80,000 people in the U.S. died from opioid overdoses. That’s not a statistic. That’s 80,000 families shattered. The CDC declared this a public health emergency in 2017 - and it’s still going.
It didn’t happen overnight. Doctors prescribed opioids too freely for years, believing the risk of addiction was low. We now know that’s false. Even short courses - just three days - can lead to dependence. A 2023 study found that patients on sustained-release oxycodone had a lower risk of overdose and death than those on morphine. But that doesn’t make oxycodone safe. It just means some opioids are slightly less dangerous than others. Still dangerous.
And it’s not just about illegal drugs. Most opioid overdoses start with a prescription. People take them longer than needed. They run out. They get desperate. They turn to street drugs like fentanyl - which is 50 times stronger than heroin. One pill can kill.
What Do the Experts Say Now?
The guidelines have changed. Big time.
The CDC’s 2022 clinical guideline says this clearly: Use non-opioid therapy as the preferred treatment for subacute and chronic pain. Opioids? Only if other options fail - and even then, start low, monitor closely, and combine them with physical therapy or other non-drug treatments.
The American College of Physicians, the VA, and the California Medical Board all say the same thing: non-opioids first. For chronic pain, opioids should be a last resort, not a first step.
Even the FDA is pushing new non-opioid drugs. Journavx, approved in 2024, is the first new class of non-opioid painkiller in decades. It works differently than NSAIDs or acetaminophen - targeting a specific pain pathway without affecting the brain’s reward system. In trials, it reduced pain better than placebo. And it didn’t cause drowsiness, constipation, or respiratory depression - the deadly side effects of opioids.
When Might Opioids Still Be Needed?
They’re not evil. They’re tools. And like any tool, they have a place.
For someone with terminal cancer, opioids can mean the difference between suffering and comfort. After major surgery - like a hip replacement - a short course (three to five days) can help manage intense pain while the body heals. In those cases, the benefits outweigh the risks.
But for lower back pain? Arthritis? Headaches? Migraines? No. The evidence doesn’t support it. The risks do.
What Should You Do If You’re on Opioids?
If you’ve been on opioids for more than a few weeks, talk to your doctor. Don’t stop cold turkey - that can cause severe withdrawal. But ask: Is this still necessary?
Ask about tapering. Ask about non-opioid alternatives. Ask about physical therapy, acupuncture, or cognitive behavioral therapy. These aren’t “alternative” - they’re evidence-based. And they work.
Keep your meds locked up. Never share them. And if you’re worried about dependence - tell someone. You’re not weak for needing help. You’re smart for asking.
What Can You Use Instead?
Here’s what actually works for most people:
- Acetaminophen (Tylenol): Good for mild to moderate pain. Safe if you don’t exceed 3,000 mg a day and don’t drink alcohol.
- NSAIDs (ibuprofen, naproxen): Reduce inflammation and pain. Best for arthritis, sprains, menstrual cramps. Avoid if you have kidney disease or stomach ulcers.
- Topical creams: Capsaicin, lidocaine patches, or menthol rubs can ease joint or muscle pain without system-wide effects.
- Physical therapy: Strengthens muscles, improves movement, reduces pain long-term.
- Cognitive behavioral therapy (CBT): Helps retrain how your brain processes pain. Proven to reduce chronic pain intensity.
- Journavx and other new options: If your doctor offers it, ask. It’s not magic - but it’s a real alternative to opioids for acute pain.
Most people don’t need a pill to feel better. They need movement, rest, and support.
The Bottom Line
Pain is real. But the solution isn’t always a pill - especially not an opioid. For most types of chronic pain, non-opioid treatments work just as well, with far fewer risks. And for acute pain - even in kids - they often work better.
The medical world has woken up. Guidelines have changed. New drugs are here. The old assumption - that opioids are the best answer - is outdated, dangerous, and wrong.
You don’t have to suffer. But you also don’t have to risk your life for relief. Ask questions. Demand safer options. Your body will thank you.
Are opioids ever safe for long-term pain?
For most chronic pain conditions - like back pain or osteoarthritis - opioids are not recommended for long-term use. Studies show they don’t work better than non-opioid options over time, and they carry serious risks like addiction, heart problems, and overdose. The CDC and other medical groups now advise using non-opioid treatments first. Opioids may be appropriate only in rare cases, like advanced cancer or after major surgery, and even then, only for short periods under close supervision.
Can non-opioid pain relievers work as well as opioids?
Yes. Multiple high-quality studies, including the landmark SPACE trial and pediatric research, show that non-opioid medications like ibuprofen and acetaminophen provide similar or better pain relief than opioids for conditions like back pain, osteoarthritis, and post-surgical pain. They also come with fewer side effects - no drowsiness, constipation, or risk of addiction. Even in children, non-opioids matched opioids in pain control while causing fewer adverse events.
What are the biggest dangers of opioids?
The biggest dangers are addiction, overdose, and long-term health damage. Opioids can cause physical dependence even after short use. Overdose can stop breathing - and it’s often fatal, especially when mixed with alcohol or benzodiazepines. Long-term use increases the risk of heart attack by more than 160%, and can lead to hormonal imbalances, immune suppression, and chronic constipation. The CDC reports over 80,000 opioid-related deaths in the U.S. in 2021 alone.
Is Journavx a good alternative to opioids?
Journavx is the first new non-opioid painkiller approved by the FDA in decades, and it’s designed specifically for acute pain like after surgery. In clinical trials, it reduced pain better than placebo and worked without the risks of opioids - no respiratory depression, no addiction potential, no constipation. It’s not for every type of pain, but for patients needing strong relief without opioids, it’s a major step forward. It’s meant to be used short-term, with NSAIDs like ibuprofen as backup.
What should I do if I think I’m addicted to pain meds?
If you’re taking opioids longer than prescribed, feeling like you need them to function, or have tried to quit but couldn’t, you may be dependent. Don’t stop suddenly - it can cause dangerous withdrawal. Talk to your doctor about a tapering plan. Many clinics offer medication-assisted treatment with buprenorphine or naltrexone, along with counseling. Support groups and behavioral therapy also help. You’re not alone - and help is available.
Can I use NSAIDs and acetaminophen together?
Yes, under a doctor’s guidance. Combining ibuprofen and acetaminophen is common and often more effective than either drug alone. For example, many post-surgery pain plans use both. But don’t exceed the daily limits: no more than 3,000 mg of acetaminophen and no more than 2,400 mg of ibuprofen in 24 hours. Avoid if you have kidney disease, liver problems, or a history of stomach bleeding.
Are there natural ways to reduce pain without meds?
Absolutely. Physical therapy, heat/cold therapy, acupuncture, yoga, and cognitive behavioral therapy (CBT) have all been shown to reduce chronic pain effectively. Movement is one of the best pain relievers - staying active helps prevent stiffness and builds strength that supports painful joints. Even mindfulness and breathing techniques can change how your brain interprets pain signals. These aren’t “alternative” - they’re science-backed and often covered by insurance.

Jamie Watts
November 15, 2025 AT 16:57Look I’ve seen this movie before doctors prescribing opioids like candy then acting shocked when people get hooked. The SPACE trial? Yeah that’s the one they buried for years. Non-opioids work just fine for 90% of us. I had a herniated disc for 3 years and ibuprofen plus PT got me back to lifting weights. Opioids? Made me foggy and constipated. No thanks.
John Mwalwala
November 17, 2025 AT 03:44Did you know the FDA approved Journavx after a secret lobbying push from Big Pharma? They’re just replacing one monopoly with another. The real danger? The opioid crisis was manufactured to push synthetic painkillers that can be patented. Morphine is old and cheap. Fentanyl? Profitable. And now Journavx? Same playbook. They don’t want you healing naturally. They want you dependent on their next billion-dollar pill.
Deepak Mishra
November 17, 2025 AT 13:04OMG I just read this and I’m crying 😭 my dad died from an overdose after 6 months on oxycodone for his back pain… he was just trying to live… they told him it was safe… I hate the system… why didn’t anyone warn us?? 😭😭😭
Rachel Wusowicz
November 19, 2025 AT 09:58They’ve been lying to us for decades. The pharmaceutical companies funded the studies that said opioids were safe. The doctors were paid to prescribe. The CDC? They were pressured to soften their guidelines. And now they’re pushing Journavx like it’s some miracle cure? It’s just the next step in the same game. They don’t want you to move. They don’t want you to heal. They want you to swallow. Always swallow.
Jennifer Walton
November 20, 2025 AT 09:19Non-opioids work. But they’re not always enough. The real issue isn’t the drugs-it’s the lack of access to physical therapy, mental health care, and time. People need more than a pill. They need support. And we don’t give it.
Kihya Beitz
November 20, 2025 AT 20:50Oh wow so now we’re supposed to believe the VA and the CDC? Next they’ll tell us smoking doesn’t cause cancer. I’ve been on tramadol for 8 years. I’m not addicted. I’m just… functional. You think I want to be on meds? No. But I’m not gonna sit here and let some guy in a lab coat tell me my pain isn’t real because it doesn’t fit his algorithm.
Diane Tomaszewski
November 21, 2025 AT 21:39I used to take opioids after my knee surgery. Felt amazing at first. Then I felt nothing but tired and weird. Switched to ibuprofen and heat packs. Took longer. But I felt like myself again. No fog. No guilt. Just healing. Sometimes simple is better.
Dan Angles
November 22, 2025 AT 17:58As a practicing physician with over two decades of clinical experience, I can affirm that the evidence presented in this post is both clinically sound and ethically imperative. The paradigm shift away from opioid-centric pain management is not merely a guideline-it is a moral obligation. Non-opioid modalities, including physical therapy, cognitive behavioral interventions, and novel pharmacotherapeutics such as Journavx, represent the standard of care. Prescribing opioids for chronic non-cancer pain without exhaustive non-pharmacological evaluation constitutes a deviation from evidence-based practice and exposes patients to preventable harm.
David Rooksby
November 23, 2025 AT 11:26Okay but let’s be real here-everyone knows the opioid crisis was started by Purdue Pharma and their ‘Pain as the 5th Vital Sign’ BS campaign. Doctors were getting bonuses for prescribing more. And now? Now they’re trying to sell us Journavx like it’s the holy grail. But guess what? It’s still a pill. And pills are still profit. They don’t want you to fix your back with yoga or your knees with weight training. They want you to keep buying. And if you don’t take the pill? They’ll tell you it’s ‘in your head.’ Meanwhile, the real solution-access to rehab, mental health care, and living wages-is never mentioned. Because that would cost money. And nobody’s making money off that.
Melanie Taylor
November 24, 2025 AT 03:36Thank you for this!! 💖 I’m from a small town where everyone just pops pills… my sister took opioids for 5 years for migraines and now she’s in recovery. We’re so lucky she made it. Please, if you’re on them-talk to someone. You’re not weak. You’re human. 🌸