Brain Tumors: Types, Grades, and Multimodal Treatments Explained
 Jan, 27 2026
Jan, 27 2026
Brain tumors aren’t one thing. They’re dozens of different diseases hiding under the same label. Two people with the same symptoms might have tumors that grow at completely different speeds, respond to totally different treatments, and have wildly different outlooks. That’s why understanding brain tumors isn’t just about knowing you have one-it’s about knowing exactly what kind you have.
How Brain Tumors Are Classified: Type and Grade
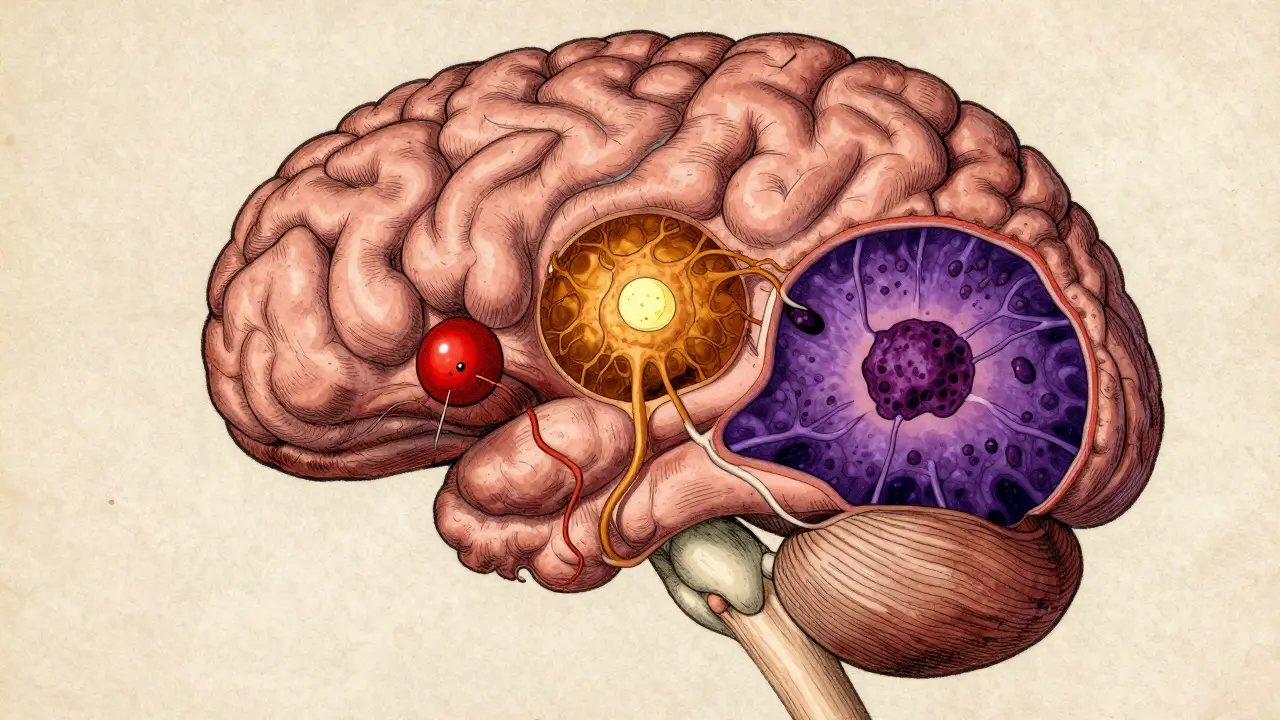
Doctors look at two main things when they diagnose a brain tumor: what type of cell it came from, and how aggressive it is. The type tells you the tumor’s origin-like whether it started in glial cells, meninges, or nerve tissue. The grade tells you how fast it’s likely to grow and spread.
The World Health Organization (WHO) sets the global standard for this. Their latest system, WHO CNS5, came out in 2021 and changed everything. Before, doctors relied mostly on how cells looked under a microscope. Now, they also test for specific genetic changes. This isn’t just a tweak-it’s a revolution in diagnosis.
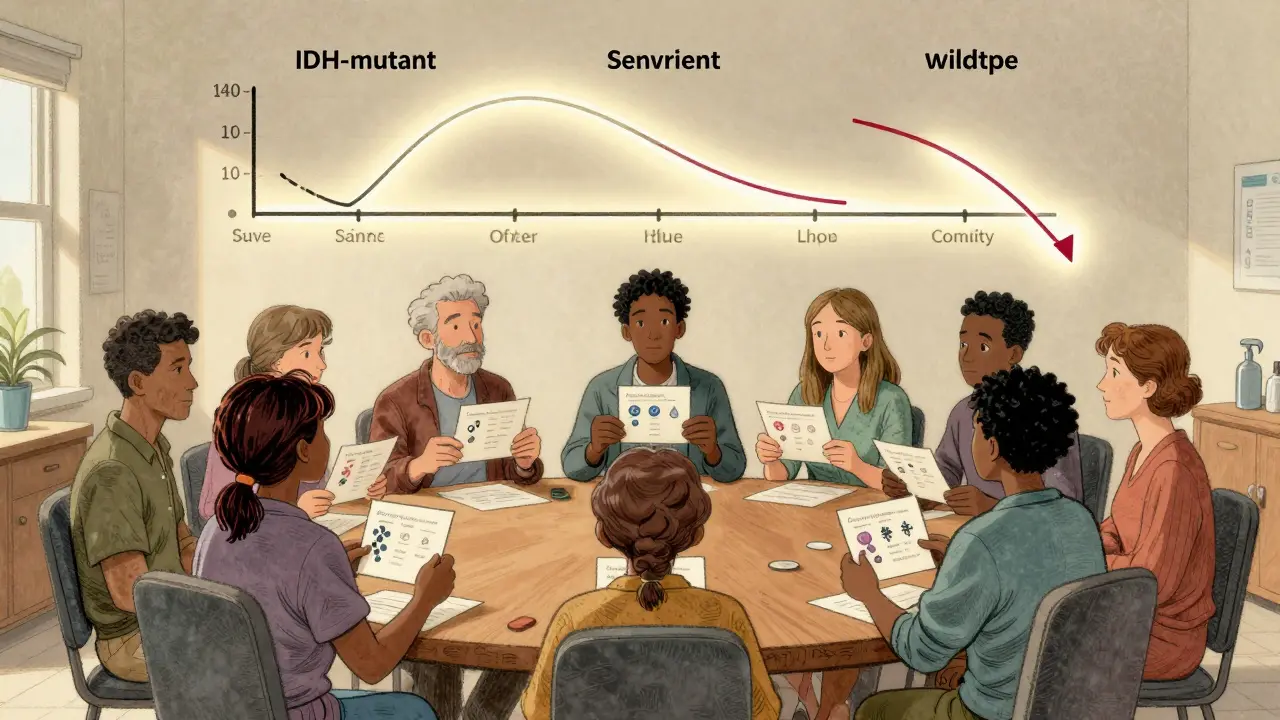
For example, two tumors might look almost identical under the microscope. But if one has an IDH mutation and the other doesn’t, they’re treated as entirely different diseases. The IDH-mutant version grows slower, responds better to treatment, and has a much longer survival rate. That’s why molecular testing is no longer optional-it’s essential.
The Four Grades of Brain Tumors
Grades range from 1 to 4, with higher numbers meaning more aggressive tumors. But here’s the catch: not all tumor types can be grade 4. Meningiomas max out at grade 3. Oligodendrogliomas only go up to grade 3. Glioblastomas? They’re always grade 4. This shift-called “within-tumor-type” grading-means doctors no longer force every tumor into the same scale. It’s more accurate.
Grade 1: These are slow-growing, often well-defined tumors. Pilocytic astrocytomas fall here. They’re usually curable with surgery alone. Patients can live for decades after removal.
Grade 2: These look almost normal under the microscope but have a sneaky habit of creeping into healthy brain tissue. Diffuse astrocytomas and oligodendrogliomas are common here. They may not spread outside the brain, but they often come back as higher-grade tumors if not fully removed.
Grade 3: These are actively growing, invasive tumors. Anaplastic astrocytomas and anaplastic oligodendrogliomas are in this group. They don’t just invade nearby tissue-they keep growing back after surgery. Radiation and chemo are usually needed right after surgery.
Grade 4: This is the most aggressive category. Glioblastoma (IDH-wildtype) makes up over half of all malignant brain tumors in adults. These tumors grow fast, form their own blood supply, and leave dead tissue in the center. Median survival with standard treatment is about 14.6 months. But if it’s an IDH-mutant grade 4 astrocytoma? Survival jumps to over 31 months.
Molecular Testing: The New Standard
What you see under the microscope is only half the story. The 2021 WHO update made molecular markers mandatory for diagnosis. Three key tests are now routine:
- IDH mutation status: If the tumor has a mutation in the IDH1 or IDH2 gene, it’s biologically different-and often less aggressive. About 80% of grade 2 and 3 gliomas have this mutation.
- 1p/19q codeletion: This genetic change is almost always found in oligodendrogliomas. It’s a good sign. Tumors with this deletion respond better to chemotherapy and have longer survival.
- MGMT promoter methylation: This doesn’t change the tumor’s grade, but it predicts how well it will respond to temozolomide, the most common chemo drug. If methylated, the tumor is more likely to shrink.
These tests take time. Labs need 7 to 10 days to run them properly. But waiting matters. A misdiagnosis based on histology alone can lead to the wrong treatment-and that can cost lives.
Thanks to new tools like the Ventana IDH1 R132H antibody, results that once took weeks now come back in 48 hours. This speed lets doctors start treatment faster, without sacrificing accuracy.
Treatment Is Never One-Size-Fits-All
There’s no single “brain tumor treatment.” What works for a grade 2 oligodendroglioma won’t help a grade 4 glioblastoma. Treatment is always multimodal-meaning surgery, radiation, and drugs are combined based on the tumor’s specific profile.
Surgery: The goal is always to remove as much as possible without damaging critical brain functions. For grade 1 tumors, complete removal can mean a cure. For grade 4, surgeons aim to reduce pressure and symptoms, knowing the tumor will return.
Radiation: Used after surgery for grades 2-4. For low-grade tumors, radiation may be delayed to avoid long-term brain damage. For high-grade tumors, it starts right away. New techniques like proton therapy help spare healthy tissue.
Chemotherapy: Temozolomide is the go-to for glioblastoma and anaplastic gliomas. But for IDH-mutant grade 2 gliomas, a new drug called vorasidenib changed the game. In the INDIGO trial, patients on vorasidenib stayed progression-free for nearly 28 months-almost triple the time of those on placebo. The FDA approved it in June 2023. This is the first drug approved specifically for low-grade gliomas based on molecular markers.
Targeted Therapy and Clinical Trials: For patients with IDH mutations, drugs like vorasidenib and ivosidenib are now standard options. Other trials are testing vaccines, immunotherapies, and gene therapies. The CODEL trial, testing combined chemo for oligodendroglioma, is expected to release results in late 2024.
What Patients Really Face
Diagnosis isn’t just medical. It’s life-changing. A 32-year-old diagnosed with a grade 2 oligodendroglioma might have 72 hours to decide whether to freeze eggs before surgery. A 60-year-old with glioblastoma might be told survival is 14 months-but if their tumor has MGMT methylation, that number could stretch to 24 months.
Patients often wait weeks for a diagnosis. One study found 68% of people waited more than 8 weeks. Those with low-grade tumors waited longer-14 weeks on average-because doctors sometimes assume they’re less urgent. But even slow-growing tumors can become dangerous if they press on speech or motor centers.
And confusion is common. A 2022 study found 42% of patients thought “grade 2” meant a 20% survival chance. It doesn’t. Grade 2 means slow growth-not terminal. Many patients live 10 to 20 years with proper care.
On patient forums, stories like “GBMWarrior87” show how molecular targeting can extend life. His IDH-mutant grade 4 tumor, treated with vorasidenib, gave him 18 months without progression-beating the standard 14.6 months. That’s not just hope. That’s science working.
Where the Field Is Headed
The future of brain tumor care is precision. Liquid biopsies-testing tumor DNA in spinal fluid-are already showing 89% accuracy in detecting recurrence. That could replace invasive scans and biopsies in the next few years.
More drugs are coming. Trials are testing drugs that target specific mutations beyond IDH, like BRAF and FGFR. Immunotherapies that train the immune system to attack tumor cells are being tested in combination with radiation.
And the grading system? It’s still evolving. The WHO has revised its classification five times since 1979. Each update has made diagnosis more accurate. The next one might include blood-based biomarkers or AI-assisted imaging analysis.
Right now, the key is this: don’t accept a diagnosis without molecular testing. If your doctor hasn’t tested for IDH, 1p/19q, or MGMT, ask why. The right treatment starts with the right diagnosis.
Survival and Outlook: What the Numbers Really Mean
Survival statistics can be scary. But they’re averages. They don’t predict your outcome.
- Grade 1 tumors: Often cured. 10-year survival exceeds 90%.
- Grade 2 tumors: Median survival is 10-15 years, but many live longer. IDH-mutant tumors do significantly better.
- Grade 3 tumors: Median survival is 5-10 years. Response to chemo and radiation improves outcomes.
- Grade 4 glioblastoma (IDH-wildtype): Median survival is 14.6 months. But with MGMT methylation, it can reach 24 months. New treatments are pushing this further.
- Grade 4 astrocytoma (IDH-mutant): Median survival is over 31 months-nearly triple the IDH-wildtype.
These numbers aren’t fixed. They’re based on past data. With new drugs like vorasidenib, survival rates are rising faster than ever.
How to Navigate the System
If you or someone you love is diagnosed:
- Ask for a copy of the pathology report. Don’t rely on summaries.
- Confirm that molecular testing (IDH, 1p/19q, MGMT) was done. If not, request it.
- Seek care at a center that treats brain tumors regularly. Academic hospitals have better access to clinical trials and advanced diagnostics.
- Connect with patient groups. The National Brain Tumor Society and Brain Tumor Foundation offer free resources and peer support.
- Consider genetic counseling. Some mutations, like IDH, can be inherited in rare cases.
Don’t rush into treatment. Take the time to get the full picture. A week of waiting for test results could mean years of better quality of life.

Kathy Scaman
January 28, 2026 AT 21:48Wow. This is the first time I’ve read something about brain tumors that didn’t make me want to Google ‘how to not die’ for 3 hours.
Phil Davis
January 29, 2026 AT 17:39So let me get this straight - we’re now diagnosing brain tumors based on gene mutations instead of just looking at cells under a microscope? Guess I should’ve majored in biochemistry instead of marketing.
Mindee Coulter
January 31, 2026 AT 03:57MGMT methylation = better chemo response. IDH mutation = longer life. 1p/19q codeletion = good news. That’s it. That’s the whole cheat sheet right there. Save this comment.
Sue Latham
January 31, 2026 AT 05:00Of course the medical elite need 10 days to run tests. They’re probably sipping artisanal matcha while waiting for the $4000 gene sequencer to warm up. Meanwhile, regular people are Googling ‘is this tumor my fault’ at 3am.
Mel MJPS
January 31, 2026 AT 10:24My cousin had a grade 2 glioma. They waited 11 weeks for molecular results. She cried every night. Then they told her the mutation was positive. She’s been in remission for 5 years now. This stuff matters. Don’t skip the tests.
Bryan Fracchia
January 31, 2026 AT 18:34It’s wild how much hope is hidden in a single gene marker. One mutation, and suddenly a death sentence becomes a slow burn. Science isn’t magic - but sometimes it feels like it.
Rhiannon Bosse
February 1, 2026 AT 08:59Let’s be real - the FDA approved vorasidenib because Big Pharma finally realized they could charge $200k/year for a pill that makes people live 18 months longer. Meanwhile, the guy who discovered it got a gold watch and a LinkedIn post.
Anna Lou Chen
February 1, 2026 AT 21:21Are we really reducing the existential horror of a brain tumor to a series of alphanumeric biomarkers? IDH-mutant. MGMT-methylated. 1p/19q codeleted. We’ve turned human suffering into a spreadsheet. The algorithm knows more about you than your mother does.
Brittany Fiddes
February 2, 2026 AT 07:41Proton therapy? Liquid biopsies? This is all very British. In the US, if you can’t afford a neuro-oncologist who moonlights as a crypto influencer, you’re just a statistic with a pulse.
Irebami Soyinka
February 2, 2026 AT 13:32USA thinks it's the only one doing real science? 😂 In Nigeria, we have doctors who diagnose brain tumors by smelling the patient’s sweat and asking about their dreams. 1p/19q? More like 1p/19q-why-are-you-so-privileged? 😆
Lexi Karuzis
February 2, 2026 AT 19:25Wait… if molecular testing is mandatory, why do 42% of patients still not get it? Who’s hiding this? Hospitals? Insurance companies? Are they afraid people will start asking for their money back if they’re misdiagnosed? Someone’s lying. I know it.
fiona vaz
February 3, 2026 AT 16:43If you’re reading this and you’ve just been diagnosed - breathe. You’re not a statistic. You’re not your grade. You’re not your mutation. You’re someone who gets to fight - and now you know exactly what weapons you have. Take the time. Get the tests. Find your team. You’ve got this.